Christina Horvath
Social Programs Coordinator
June 30, 2024
Success of the Alzheimer Society’s Grant-Funded Project
The Alzheimer Society is excited to share the success of our recent grant-funded project aimed at supporting care partners of persons living with dementia. Our ‘Journey to Self-Care: Supporting Those Who Support Others’ retreats have provided invaluable resources, education, and emotional support to caregivers to help them manage stress and improve their overall well-being. As a Social Programs Coordinator, I led the creation and execution of this event. Witnessing the positive impact of these retreats has been incredibly rewarding.
Importance of Care Partners
Care partners are critical to the quality of life of those living with dementia. Care partners assist with everyday activities, coordinate medical care, and provide psychological support, companionship, and advocacy (Alzheimer Society of Canada, 2022). By 2050, the number of care partners in Canada is expected to exceed 1 million (Alzheimer Society of Canada, 2022). Adult children (58%) and spouses (32%) comprise the majority of unpaid care partners (CIHI, 2018b).
Unique Challenges
Both subgroups face unique caregiving challenges (Alzheimer Society of Canada, 2022):
- Adult Children:
- Significant impacts on work and economic stability as they balance caregiving with career and familial responsibilities.
- Spouses:
- Heightened stress while managing their own health issues.
There is also a gender-based bias, with women representing almost 54% of the caregiving population.
Physical and Emotional Strain
Care partners are referred to as ‘invisible second patients’ due to the toll on both their physical and emotional health from providing hours of care (Richardson, 2013; Zhu et al., 2014).
Care partners often express feelings of anger at the dementia diagnosis, sadness over the loss of relationship, and guilt considering long-term care (Brodaty & Donkin, 2009). Loss of control over the future and ‘feeling trapped in a caregiving role’ contribute to high rates of burden, social isolation, physical ill-health, and financial hardships (Brodaty & Donkin, 2009).
- Distress Symptoms: 45% of care partners exhibit distress symptoms (CIHI, 2018b)
- Inability to Continue Caregiving: 21% feel unable to continue caregiving due to stress (CIHI, 2018b).

“You’ve taken us out of the isolation that dementia can cause and reminded us to laugh, feel supported and live our best life.” – Mary (Care Partner)

“It was good to hear everyone else’s story and it made me feel “less alone” on this journey. Also, I wanted to thank you for allowing us to take one of the knitted items [Twiddlemuffs] for our loved ones. My mom really liked it and even I was surprised.” – Rita (Care Partner)




Retreat Components
Our retreats were crafted to equip care partners with the essential tools and supportive environment necessary to empower them on their caregiving journey. Care partners were organized into small, rotating groups based on their relationship to their person living with dementia such as spouses (male and female) and adult children. This approach facilitated intimate, purposeful groups where care partners could connect with others in similar situations, nurturing meaningful relationships and reducing feelings of isolation. The event centered around three main components:
- Education:
- Focus on stress management and balancing caregiving responsibilities.
- Comprehensive education on how stress affects the body and the burden of caregiving.
- Strategies to find balance and encouragement to create a ‘Care Partner Team’ to share caregiving responsibilities.
- Counselling and Behavioural Support:
- Address specific care partner concerns through intimate group sessions.
- Participants shared their questions and issues confidentially during registration, guiding our counselling and behavioural supports team.
- Encouraged open discussions about personal caregiving journeys in a guilt-free zone.
- Social Programs:
- Included therapy dogs, creative play workshop, and guided meditation.
- Partnered with Therapy Tails to provide comfort and companionship.
- Stress-relieving benefits of fun and play through charades or balloon musical chairs, sparking laughter.
- Concluded with a guided meditation session, leaving care partners refreshed and inspired to continue these activities at home.

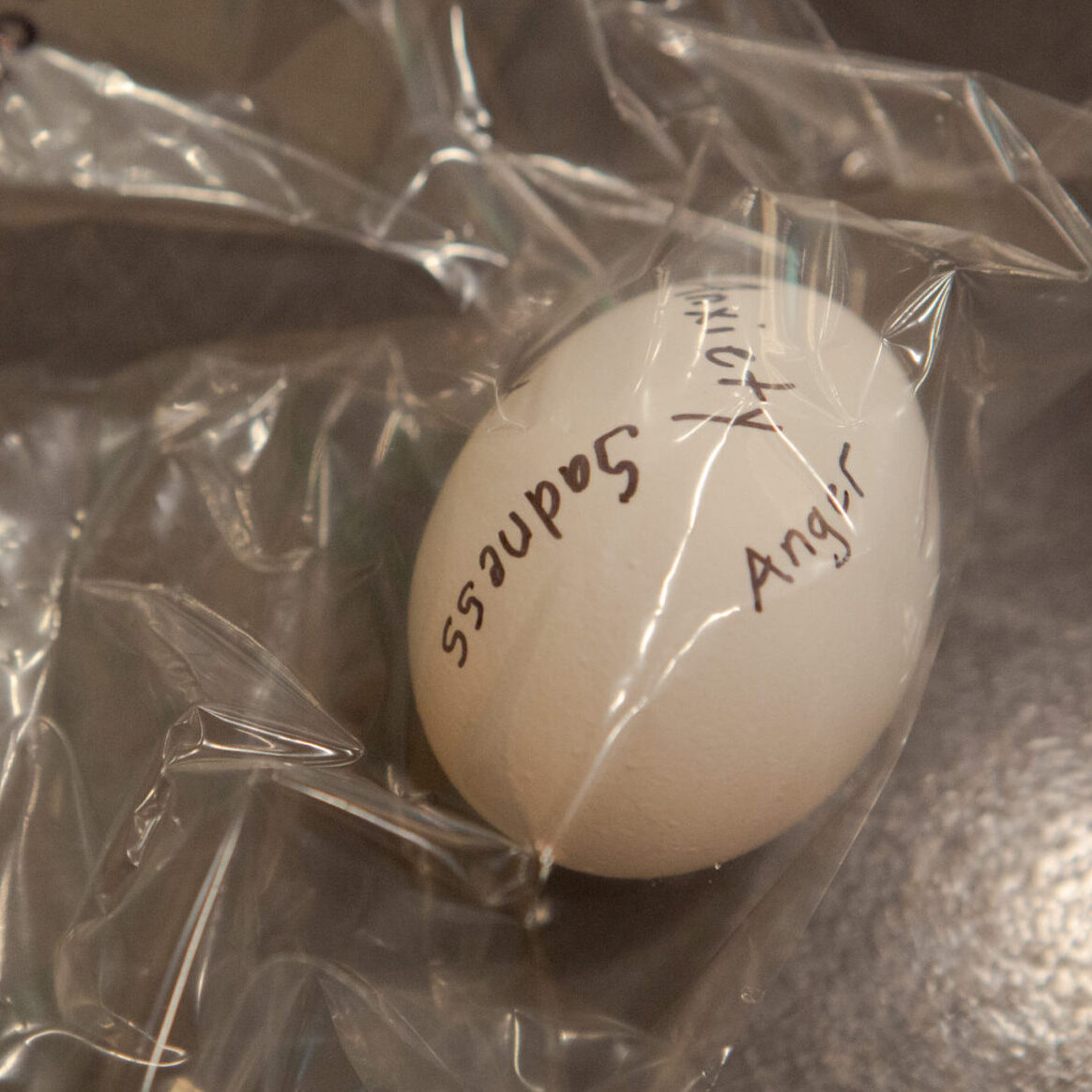


Special Activities
A meaningful activity was our egg-spression eggs. Care partners reflected on a negative emotion, wrote it on a hollowed egg, and at the end of the retreat, crushed the egg to symbolize leaving those emotions behind.
Self-Care Package
Care partners left with a self-care package that included:
- Lavender aromatherapy rollerballs: the lavender scent is relaxing; it is often used to aid in relieving stress, anxiety, and promoting good sleep.
- Korean skin care mask
- Unique affirmation card
- Shower steamer
- Stress ball
Future Aspirations
At the Alzheimer Society, we aspire to support not only those living with dementia but also their care partners and families. Through initiatives like our ‘Journey to Self-Care’ retreats we aim to enhance the well-being of care-partners.
Why This Matters
Supporting care partners with education, emotional support, and practical tools helps them manage significant stress and challenges associated with caregiving. When care partners are better equipped and less stressed, they are more capable of providing sustained, high-quality care at home. Thus, delaying the need for institutional care, allowing persons living with dementia to remain in familiar and comfortable environments longer. Improved care partner well-being directly contributes to:
- Reduced Burnout
- Enhanced Coping Skills
- Improved Physical and Mental Health
Looking forward, we are committed to expanding our support networks and services to ensure caregivers receive the assistance they need to navigate their journey with resilience and hope.

“Facilitating a session for care partners of loved ones with dementia was incredibly meaningful, as it provided a supportive environment for sharing experiences and strategies. Witnessing their resilience and mutual support underscored the profound impact of community and understanding in navigating such challenging circumstances.” – Anisha Deol (Counsellor)

Acknowledgments
Special thanks to our team: Cathy Ryan (Counsellor), Gail Tomaselli (BSO), Anisha Deol (Counsellor), Andrew Amatiello (BSO), Darcy McKellar (Counsellor), Katharine Champaigne (PEC), Mahitab Desoky (Lead Event Volunteer), Gabrielle Rabbat (Event Volunteer), Tess Potter (Event Volunteer), and Maryam Yahya (Event Volunteer). Their efforts and kindness were instrumental to the success of each retreat.
A special shoutout to the Courtyard Marriott in Hamilton for hosting our events, with Rachael Wills and Rob Mancione going above and beyond to cater to our needs.


Left: Mahitab Desoky (Lead Event Volunteer) Right: Christina Horvath (Social Programs Coordinator)
References:
Alzheimer Society of Canada. (2022). Alzheimer Society of Canada: Navigating the Path Forward for Dementia in Canada: The Landmark Study Report #1. https://alzheimer.ca/sites/default/files/documents/Landmark-Study-Report-1-Path_Alzheimer-Society-Canada_0.pdf
Brodaty, H., & Donkin, M. (2009). Family caregivers of people with dementia. Dialogues in clinical neuroscience, 11(2), 217-228.
Canadian Institute for Health Information. (2018b). Unpaid Caregiver Challenges and Supports | CIHI. https://www.cihi.ca/en/dementia-in-canada/unpaid-caregiver-challenges-and-supports#admission
Richardson, T. J. (2013). Caregiver health: Health of caregivers of Alzheimer’s and other dementia patients. Current psychiatry reports, 15(7). https://doi.org/10.1007/s11920-013-0367-2
Zhu, C. W., Scarmeas, N., Ornstein, K., Albert, M., Brandt, J., Blacker, D., Sano, M., & Stern, Y. (2015). Health-care use and cost in dementia caregivers: Longitudinal results from the Predictors Caregiver Study. Alzheimer’s & Dementia, 11(4), 444–454. https://doi.org/10.1016/j.jalz.2013.12.018